Case studies
These case studies, developed with carers, address different situations where social work can offer input to carers. Each has information about the situation and case records, and highlights important topics that relate to that situation with questions for practice.
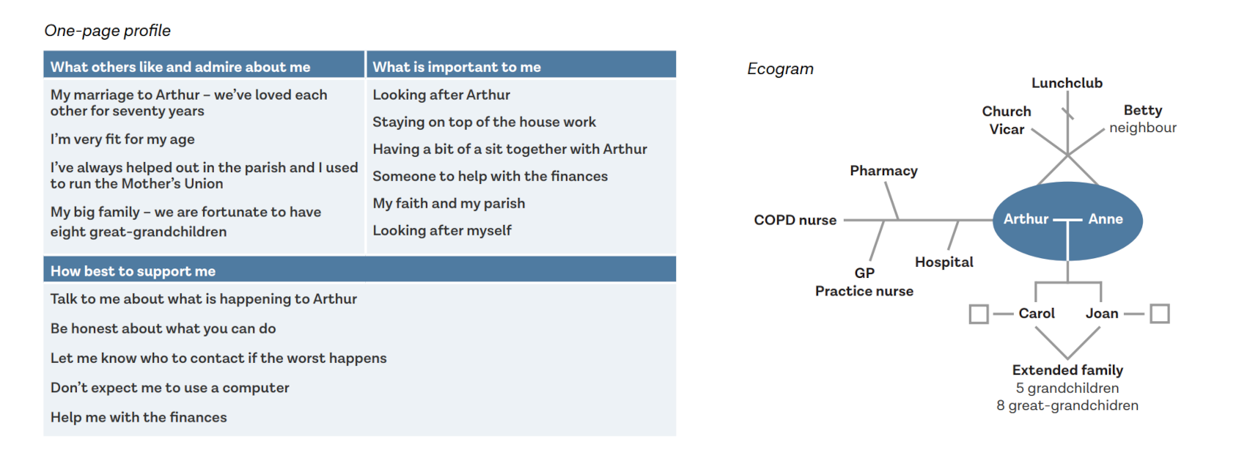
About Anne
We have always said we would stay together till the very end. That is all I want, to be together in our own home.
Anne has been married to Arthur for over 70 years. Arthur has end-stage Chronic Pulmonary Disease and is nearing the end of his life.
Read more about Anne's story below.
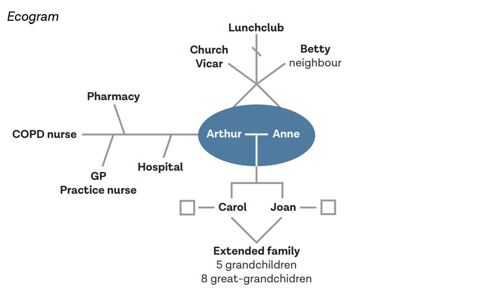
Anne Woolsey is married to Arthur, 94. They have been married for over 70 years and live in their own bungalow in a village. Anne and Arthur have two daughters, five grandchildren and eight great-grandchildren. The family are quite dispersed across the country. Their nearest daughter Carol, who lives 40 miles away, visits twice a month. Daughter Jean visits every other month. Both daughters phone regularly. Their neighbour Betty calls in most days.
Arthur has end-stage Chronic Pulmonary Disease (COPD) and is nearing the end of his life. Arthur is currently housebound, using oxygen at home. He has support from a Community COPD nurse. Anne has provided care for Arthur for eight years, and the support that he needs is increasing. The COPD affects Arthur’s mobility and he is unable to get to the toilet in time at night. Most mornings he awakens with soiled sheets which distresses him. Anne continues to look after the home and has started to manage the finances, which previously Arthur did. Anne and Arthur find it difficult to talk with each other about Arthur’s death. They would both like Arthur to die at home, with his wife and daughters.
Anne’s health is generally good, though she has mild arthritis and takes tablets for angina. However, she is becoming less strong and more tired. Anne has some hearing impairment and finds it difficult to read small print. Anne devotes her time to caring for Arthur and no longer goes to church. Both were previously active in the community and attended a local lunch club. Anne is determined to be there for Arthur and does not like to leave him, even with someone else. Her main concern is that she will not be able to support Arthur till the end. Anne is beginning to find it difficult to look after the home and garden, and to feel quite isolated. She is not confident in managing the family finances and is not sure how she will manage when Arthur is gone.
Carol is concerned about her mother not sleeping well and looking tired. She rings the local authority.
You are the social worker, and go out to see Anne and Arthur.
- What potential is there in the Care Act 2014 to support Anne flexibly as things change?
-
How can you develop integrated support for the family in this end-of-life phase?
-
How can social work’s therapeutic role support Anne and Arthur?
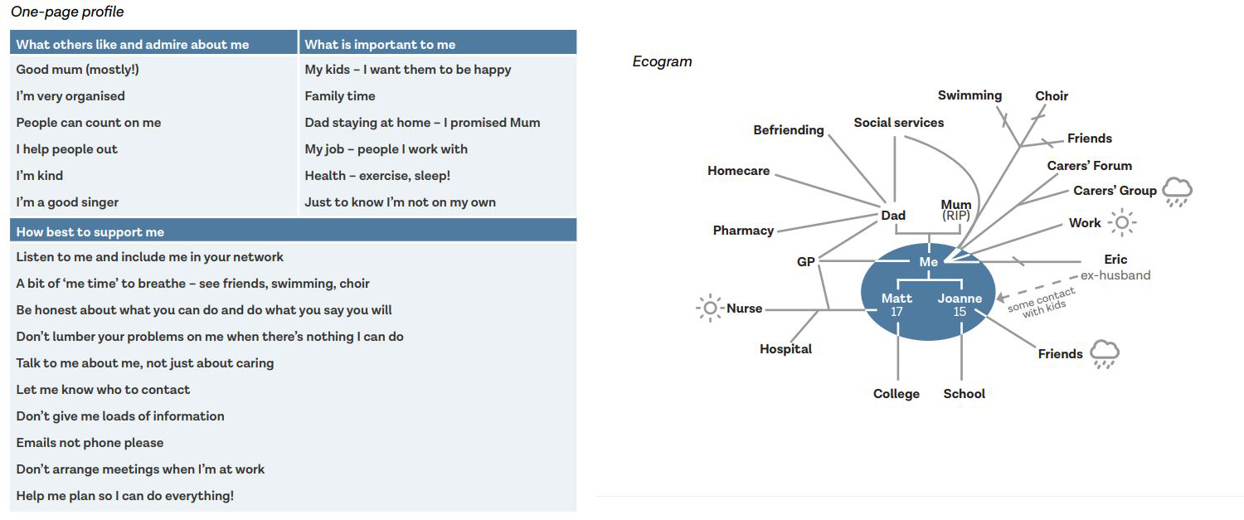
About Eve
It’s my choice to care for my family and I want to keep on doing that, and be a good mum and a good daughter.
Eve is a carer for her father, who has early-stage vascular dementia and numerous health problems. She has two children: a son, Matt, who is 17 and has Crohn’s disease, and a daughter, Joanne, who is 15.
Read more about Eve's story below.
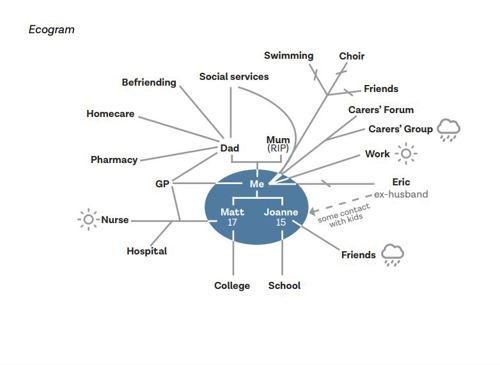
Eve Davies lives in a town. She has two children, a son, Matt, who is 17 and has Crohn’s disease, and a daughter, Joanne, who is 15. Eve’s mother died four years ago, and her father, Geoff, lives close by. Geoff is living with early stage vascular dementia and numerous health problems relating to a heart attack he had two years ago. Eve works part time in an administration role at a local college. She has lost contact with her friends and lost touch with her hobbies (swimming
and singing in a choir) because she has prioritised her family.
Matt is at college studying for his A levels. He is frustrated that his illness is interfering with all aspects of his life. Joanne is becoming more withdrawn and resentful as an increasing amount of Eve’s time is taken up with other family members. Geoff often forgets to eat or wash, and is finding it more difficult to carry out daily tasks. Following a social care assessment, he has a befriending service stop by every week and a homecare team each morning to check he’s ok and supervise his medication, which Eve sets up for them. The care agency have reported that there’s a possibility Geoff has been accessing his medication and taking it. Geoff remains adamant that he is fine, and with Eve’s support he can manage.
Eve is feeling stressed and isolated. She wants to increase her working hours for financial reasons, but is unable to as she needs to be available for Geoff. Eve is having problems with sleeping and feels generally run down, and recently has been suffering from stomach pain and nausea. She says that she feels ‘withdrawn from normal life.’ She tried attending a carers’ group but found that listening to other carers’ problems highlighted her own. Instead, she sometimes uses an online forum at night when everyone else is asleep.
Eve was recently referred by her GP for a carer’s assessment.
You are the social worker and go to see Eve.
-
How can the Care Act 2014 duty to assess how far a carer is willing and able to care empower Eve?
-
How can a whole family approach help everyone to understand and respond to this situation?
-
What does a strengths-based approach look like for someone living with dementia?
About George
Just tell me what help is out there and I will get it sorted.
George helps out their friend David who lives 150 miles away across the Welsh border. David has depression and has been in and out of hospital.
Read more about George's story below.
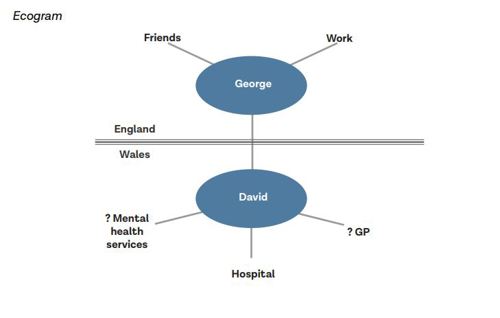
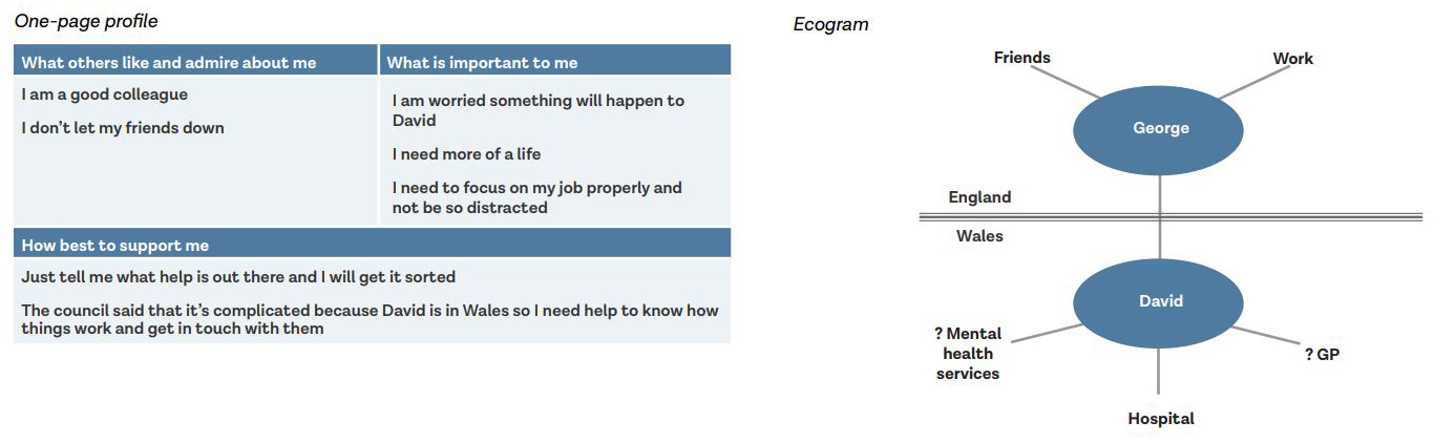
George Cook and David Taylor grew up in the same small border town and went to the same all-boy’s school in Wales. George moved away to London and became a lawyer. They are nonbinary (pronouns they, them), and have a busy work and social life. David was diagnosed with depression when he was in his late 30s. He lives alone and is often unemployed, and is a regular drug user. David’s parents are both dead and his friends have drifted away, apart from George.
George loves their childhood friend and wants to make sure he is ok. They go back to visit David every 4-6 weeks, whenever work allows. It is a 3 hour trip each way, and George usually stays overnight, tidies up, encourages David to go out for a walk, and brings shopping and anything David needs. George usually gives David some money, though they worry what David might spend it on.
George is finding the physical toll of the visits is getting too much. The greatest impact, though, is emotional. David sends frequent messages, including through the night, and George doesn’t feel able not to respond. At times, the messages are very low and George will call and be on the phone for hours. One time, David did not answer and George drove to see him, missing an important work meeting.
George has no idea what would help. They have called the council and said they need to talk to someone who knows about social services. The person they spoke to said that they could talk to a social worker to get some advice but it is complex because David lives in Wales.
You are the social worker and arrange a video call with George.
-
How can you ensure that borders are not a barrier to good social work?
-
How can you support George to have the relationship that they want with their friend?
-
How can you help people to balance risk enablement and risk management?
About Jake
It’s lonely and I could do with somewhere to let off steam.
Jake supports his second wife Deborah, who has Parkinson’s. He does not see himself as a carer.
Read more about Jake's story below.
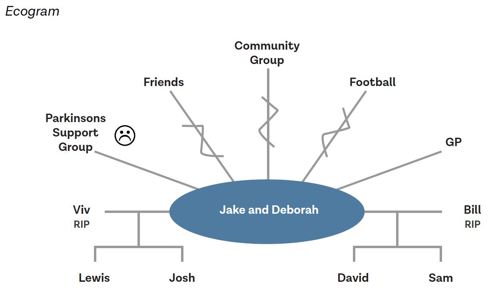
Jake Adler is 63 and looks after his wife Deborah. Deborah was diagnosed with Parkinson’s two years after they got married. They were both widowed and met through the Jewish community group. They each have two sons, who visit regularly, as well as friends and neighbours that they see often.
Over the last year, Deborah has found it increasingly difficult to leave the house and is reluctant to have visitors. Jake has gradually given up his social activities and has not renewed his season ticket for the football.
Jake was an engineer so he has done some DIY in their home to make things easier for Deborah. He provides all the physical help that she needs and manages everything in the home. Jake has taken pride in not asking anyone for help. A few months ago, a friend suggested that he went along to a support group for family of people with Parkinson’s. Jake found that most people there were women and that he didn’t want to talk about Deborah’s illness. He just wanted someone to talk to about the things he was interested in.
Deborah has become more withdrawn and Jake misses her even though she is there. The social network had been maintained by Deborah and so they are now falling out of touch with people.
One of the neighbours suggested that Jake ask the council about a ramp to get in and out of the house, and so he phoned up and agreed to a carer’s assessment.
You are the social worker and arrange to meet Jake in a café to talk.
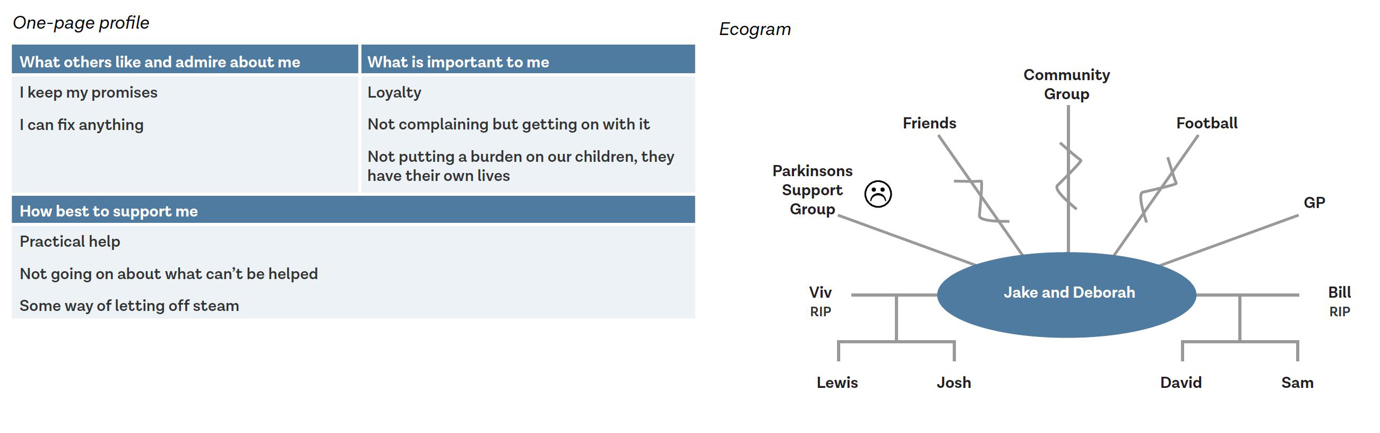
- How can social work empower people as carers if they do not see themselves as having this role?
- How do gender differences and socially configured roles affect the experiences of caring?
- What is the social work role in tackling loneliness?
About Josef
I’d like some free time on my own to have time to myself or go out with friends. I need someone to talk to about mum.
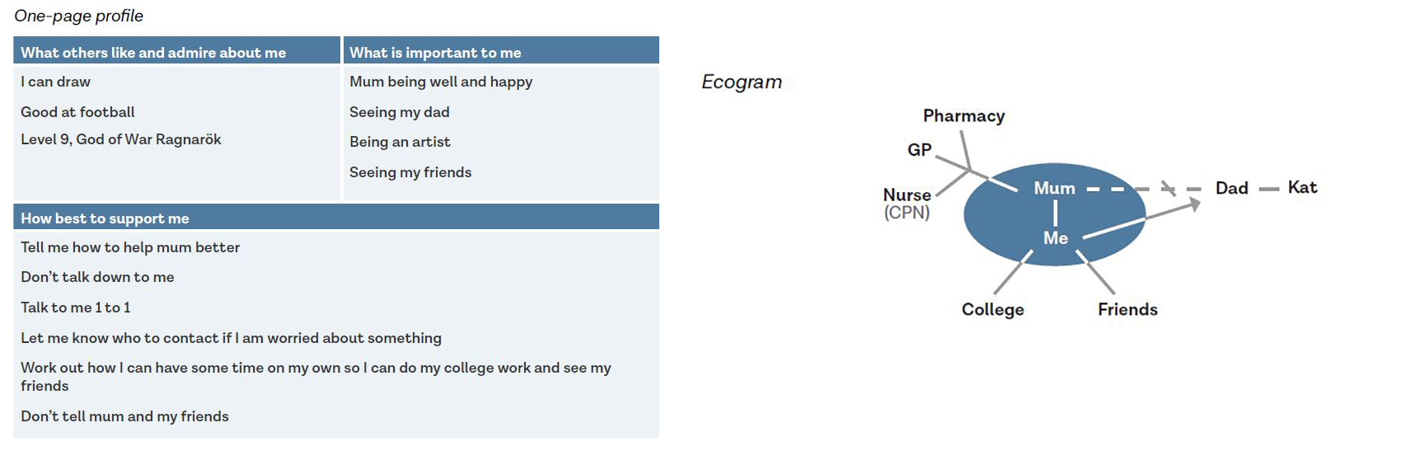
Josef is 16 and lives with his mother, Dorota, who was diagnosed with Bipolar disorder seven years ago. Josef was born in England. His parents are Polish and his father sees him infrequently.
Read more about Josef's story below.
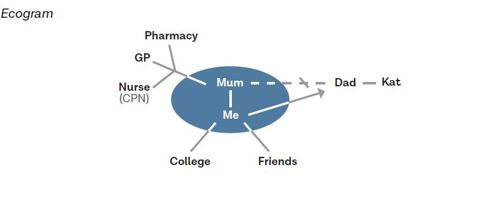
Josef Mazur lives in a small town with his mother Dorota who is 39. Dorota was diagnosed with Bi-polar disorder seven years ago after she was admitted to hospital. She is currently unable to work. Josef’s father, Stefan, lives in the same town and he sees him every few weeks. Josef was born in England. His parents are Polish and he speaks Polish at home.
Josef is doing a foundation art course at college. Dorota is quite isolated because she often finds it difficult to leave the house. Dorota takes medication and had regular visits from the Community Psychiatric Nurse when she was diagnosed and support from the Community Mental Health team to sort out her finances. Josef does the shopping and collects prescriptions. He also helps with letters and forms because Dorota doesn’t understand all the English. Dorota gets worried when Josef is out. When Dorota is feeling depressed, Josef stays at home with her. When Dorota is heading for a high, she tries to take Josef to do ‘exciting stuff’ as she calls it. She also spends a lot of money and is very restless.
Josef worries about his mother’s moods. He is worried about her not being happy and concerned at the money she spends when she is in a high mood state. Josef struggles to manage his day around his mother’s demands and to sleep when she is high. Josef has not told anyone about the support he gives to his mother. He is embarrassed by some of the things she does and is teased by his friends, and he does not think of himself as a carer. Josef has recently had trouble keeping up with course work and attendance. He has been invited to a meeting with his tutor to formally review attendance and is worried he will get kicked out. Josef has some friends but he doesn’t have anyone he can confide in. His father doesn’t speak to his mother.
Josef sees some information online about having a parent with a mental health problem. He sends a contact form to ask for information. Someone rings him and he agrees to come into the young carers’ team and talk to a social worker.
You are the social worker and have a meeting with Josef.
- How can a human-rights approach empower Josef?
- What social work capabilities are needed to build a relationship with Josef?
- What considerations are there around capacity, confidentiality and consent?
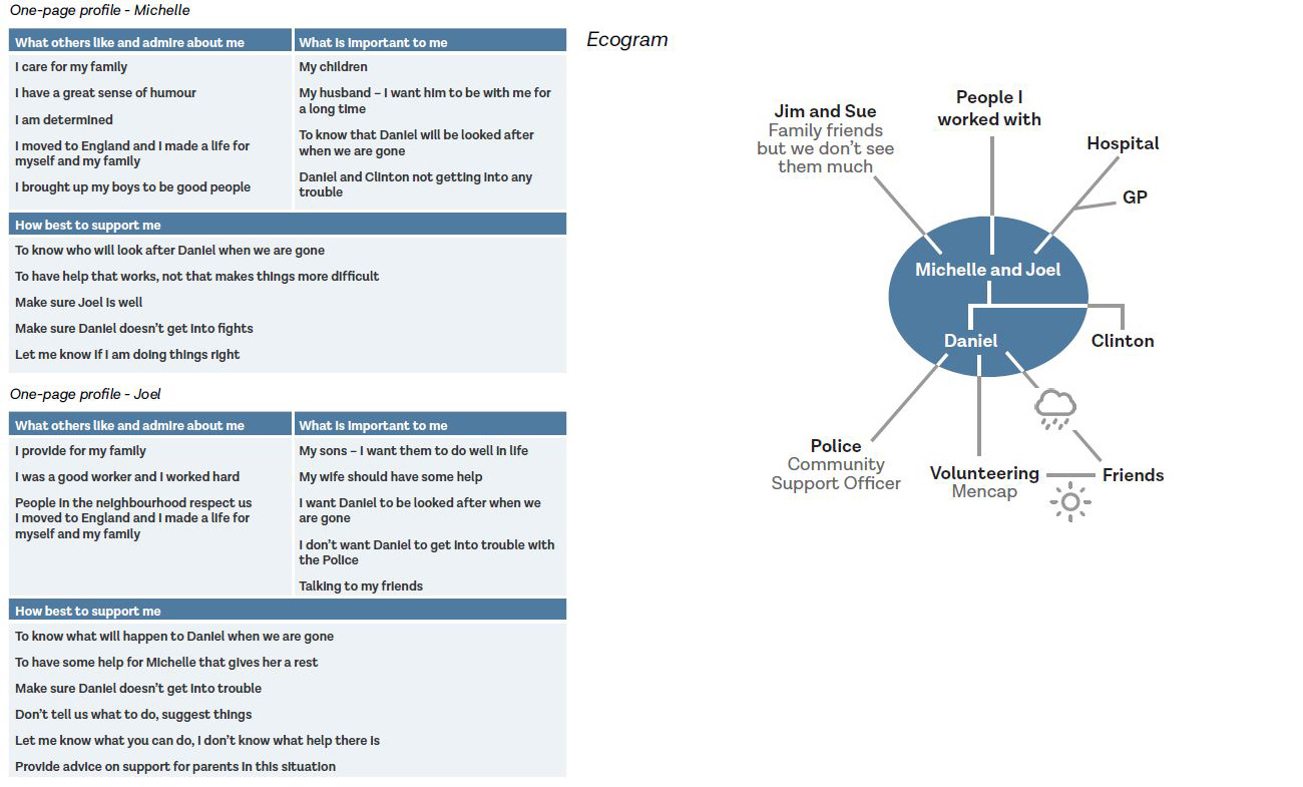
About Michelle and Joel
We need to know what will happen when we can’t look after Daniel.
Michelle and Joel have been married for 45 years and have two sons, Clinton in Scotland and Daniel, who is 34 and lives with them. Daniel has a learning disability.
Read more about Michelle and Joel's story below.
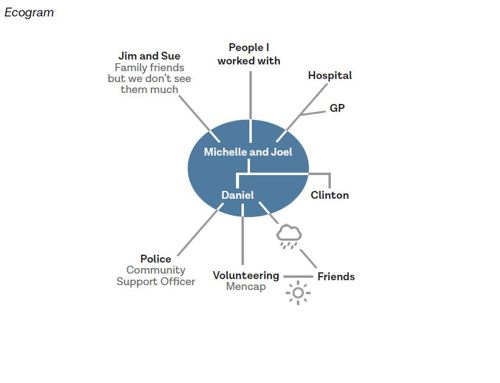
Michelle and Joel Tyndell live in a city. They were both born in Kingston, Jamaica, and moved to the United Kingdom in the 1970s just after they were married. They have been married for 45 years and have two sons, Clinton in Scotland and Daniel, who is 34 and lives with them. Daniel has a learning disability. Michelle gave up work when Daniel was 16 to support him. Joel retired three years ago. Over the years they have sought support through the council but it has never worked very well.
Daniel volunteers at a local charity a few days a week, helping with teas and coffees. He would like to live independently. Joel and Michelle are worried this won’t work. Daniel is well known in the local community. He is also known to the police due to a few incidents where he has been violent. Daniel is often misunderstood as it is not immediately clear that he has a learning disability, and people who don’t know him can react to his behaviour. This is made worse by racist stereotyping also affecting how people react to him. Daniel has some friends from volunteering and some other friends from the local area.
Joel and Michelle support Daniel to ensure he is washed and dressed appropriately, has had his medication and knows where he needs to be. Sometimes Daniel refuses his medication. Daniel has a mobile phone which he is able to make and receive calls on. Sometimes Michelle drives Daniel and sometimes they take him to the bus. Daniel has his own money but it is not clear what he is spending it on. Michelle and Joel are concerned that Daniel may be giving money to his friends.
Joel and Michelle love their son, however they are exhausted and feel undervalued by providing his care. They have had to make choices to put Daniel first, have few friends and rely on each other. Joel had a heart attack last year and they are fearful about what will happen with Daniel in the future. Before children, Michelle and Joel were keen music fans.
Michelle and Joel recently rang the council and asked for someone to talk to them about their situation.
You are the social worker go out to see Michelle and Joel.
- How does the Care Act 2014’s duties around preventing needs help you to plan for the future?
- How can you balance the needs of the different family members involved?
- How can you ensure your practice is sensitive to any cultural difference?
About Muhammed and Maryam
I want to fulfill my responsibility to my daughter.
Muhammed and Maryam have one child Layla who is 17 years old. Layla was born with Spina Bifida and has been attending a residential college.
Read more about Muhammed and Maryam's story below.
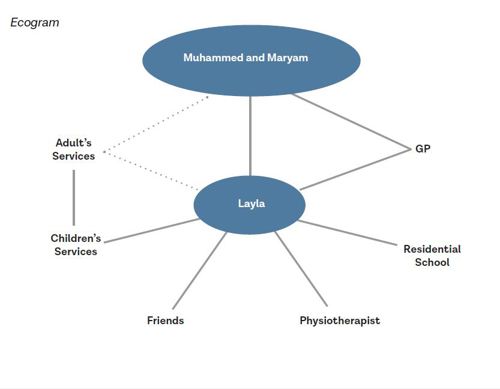
Muhammed and Maryam Hossain live on the edge of a large city. Muhammed’s parents came to the UK from Bangladesh in the 70s and he was born here. He married Maryam from Bangladesh 25 years ago and she came to live in the UK then. They have one child Layla who is 17 year’s old. Layla was born with Spina Bifida. She uses a walking aid and has an electric wheelchair. Layla has been attending a residential college where she has made good friends. She hopes to keep studying and to move in with friends.
Muhammed and Maryam want to support Layla and also to ensure that she is safe and her religion (Islam) is respected.
Muhammed and Maryam are conscious that people they know through the college had a difficult experience when their children turned 18. They want to ensure that Layla has the right support and opportunities, and to start planning for that now. They don’t have any savings themselves. Muhammed’s job is not well paid and they don’t have a house of their own. Recent increases in bills have made it difficult for them to manage when Layla comes home as the house needs to be warmer and they use more electricity.
Muhammed rang the council and asked to speak to a social worker.
You are the social worker and go out to visit them with an interpreter as Maryam finds complex topics in English difficult.

- How does the Care Act 2014’s duties around transition help you to empower this family?
- How can you ensure that both carers are fully involved and their needs are considered?
- What is the social work role in promoting economic wellbeing?
About Susan
I’d like someone to discuss my concerns with and talk things through, so I feel reassured I am making the right choices, for both of us. I must get it right.
Susan is the carer for her partner Grace who is 82. Grace has become increasingly frail and, following hospital admission and rehabilitation, has agreed to a trial for three months in a care home.
Read more about Susan's story below.
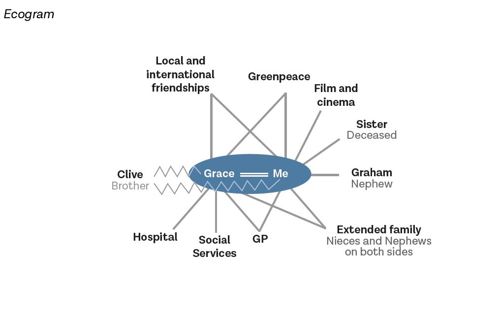
Susan Reinfeld is 70 years old. She is primary carer for her partner, Grace Wilson, who is 82. In their younger days Susan and Grace travelled widely, they had a large network of friends and although they don’t have any children of their own, they have nieces and nephews. Susan is particularly close to her nephew Graham. Grace has generally taken the lead in decisions and in the relationship. Sometimes now she gets angry with Susan if she doesn’t do things the way Grace expects or if Susan makes a suggestion that Grace sees as ‘stupid.’ Grace’s family has at times struggled with her sexuality and while her relationship with her nieces and nephews is good, her relationship with her brother Clive has been more difficult.
Over recent years Grace has become increasingly frail and has relied on Susan to get washed and dressed, and use the toilet, as well as maintain the home and cook meals. Two months ago, Grace had a fall and was admitted to the hospital. She was discharged to a rehabilitation bed in a care home. Before the hospital admission Susan and Grace were not in contact with services. Whilst in hospital and the care home, Susan has visited every day and helped Grace with personal care. Grace frequently phones and texts Susan. After six weeks of rehabilitation, Grace continues to need support to walk and with all her personal care, including support at night. You have been involved in a multi-disciplinary assessment which has recommended that Grace needs 24-hour care. As part of this assessment, Susan talked about how exhausted she is, and said that she no longer feels able to support Grace at home because of the impact on her health. Grace has agreed to a trial three months in a care home.
Susan and Grace are not legal partners, as they have not entered into a civil partnership nor are they married. Susan has no power of attorney for Grace. Susan is worried about the costs of a home and how this will be paid for. She feels guilty about ‘letting Grace down’ and sad about the future she will no longer have with Grace. Susan is also worried about Clive’s reaction.
Susan has asked to speak to someone about her concerns.
You are the social worker and go to meet Susan.
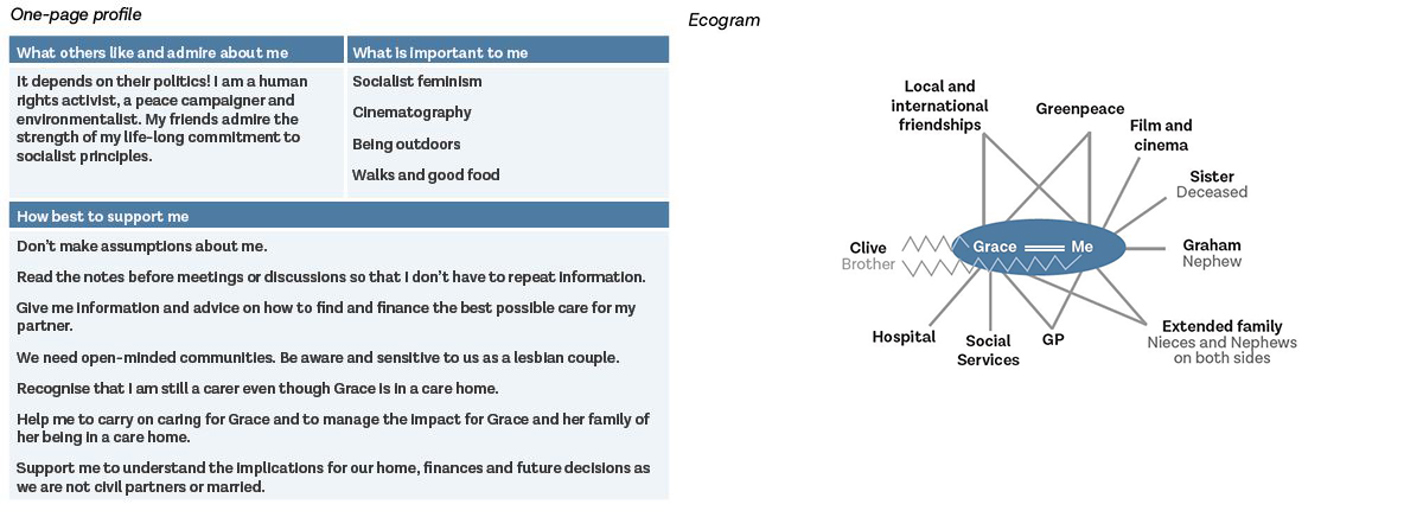
- How can a human rights perspective help you to empower Susan and Grace?
- How can you act as a navigator to make the systems around Susan and Grace transparent and understandable?
- How does an intersectional view of Susan’s and Grace’s identities (seeing the overlapping aspects of identity) help you to understand how they respond to social care?
